National Eye Care Recovery and Transformation Programme
4 May 2021
Over recent years the NHS has been seeking to reform care through pathway and service integration. Pre 2020 this was via the National Outpatient Transformation Project which commenced in 2018/19. As the covid pandemic impacted on the UK and NHS throughout 2020 the project evolved to be come part of the National Pathway Improvement Programme.
The NHS pathway improvement program brings together all NHS improvement programmes and aims to avoid duplication of effort, by coordinating resources so that transformation is delivered across the whole pathway. Eyecare pathway transformation will be the vanguard for NHS transformation via the National Eye Care Recovery and Transformation Programme.
The programme has three core high level aims:
- To improve experience, outcomes, safety and quality of care for patients in a sustainable and efficient way.
- Set out a bold but grounded digital approach to transforming eye care, to improve clinical outcomes, patient experience and productivity.
- In so doing, create a replicable model for NHS digital transformation, focussed on what opportunities for improvement to embrace, and how to scale their adoption across a federated system.
The programme will initially deliver intensive support to three systems in order to test and learn with a view to wider delivery. The identified systems are:
- North Central London ICS
- Greater Manchester ICS
- TBC
In parallel, and to scale beyond the three pilot ICSs, all systems will be provided with a suite of resources to inform their recovery planning for eye care. The programme will build capability in the regional teams and will be supplemented by national expertise as needed. This will create a national ‘community of practice’ to share learnings, standards, patterns and assets in order to scale up nationally.
Agile working
The programme will adopt a digital methodology and take a digital approach to end-to-end eye care transformation, and all team members will be expected to work in an agile manner.
The programme has senior NHS leadership and will ultimately report to the National Productivity board, chaired by Amanda Pritchard, the NHS’ Chief Operating Officer (COO).
The programme has identified seven areas of work and appointed a core team and reference group for each workstream. Primary care is well-represented in each workstream. Some workstreams have commenced their work and making some early progress whist others are still forming their teams and agreeing core aims.
Programme workstreams – Optometry involvement in core team workstreams
Pathway Improvement and Recovery – Zoe Richmond
Digital Hubs – Peter Hampson
Home care – Daniel Hardiman McCartney
EeRS – Claire Roberts
Workforce Optimisation – TBC
Commissioning – Richard Whittington
Data and Analytics – Representation within the ref group
Pathway Improvement and Recovery workstream
The workstream has a range of core deliverables:
- To support systems in setting up high volume surgical hubs to improve theatre productivity and reduce the backlog of routine cases. This should be delivered via a visible elective PTL (Patient tracking list) with enough detail to understand resource requirement and risk. This will result in more co-ordination support and equity within and between ICSs, ensuring health inequalities are not created because of high flow clinics.
- To support systems/regions in implementing standardised integrated care pathways across cataracts, urgent care (CUES/MECS), medical retina and glaucoma pathways including:
- Primary, secondary, community and independent sector eye care services.
- Risk stratification for new and follow-up patients, including failsafe processes and regular recording of ECAD (earliest clinically appropriate date) to reduce harm.
- Primary care optometrists as first contact practitioners and managing low risks in the community.
A series of patient support videos are being developed. They will be short, and NHS branded covering common clinical areas, such as: Cataract surgery, Glaucoma care, emotional support services, remote care and AMD. There will be a video explaining who’s who in the eye care world (Optometrist, DO and CLO all listed) and another describing the extended primary care pathways.
Digital Hubs
The workstream core aim is to develop a scalable model of digital Eye Care Hubs that can receive clinical data from any source and respond with the clinical expertise required to support care in non-hospital settings.
Home Care
This workstream will develop a scalable model of home care monitoring using multiple channels including patient-initiated follow-up (PIFU), symptoms monitoring and video consultation.
Workforce optimisation
The workstream will be supporting systems to identify and quantify staff recruitment, training, and optimisation with planning for the delivery of eyecare across whole systems. This will include the development of a Healthcare Professionals Qualifications, Capabilities and Competence reference document and a workforce matrix tool.
Commissioning
This workstream will identify commissioning mechanisms to enable delivery.
Early discovery work has commenced with systems to gain an understanding of what the eye care transformation programme can offer systems in terms of tools and support.
Data and analytics
This work stream is working across sets of short-term and long-term aims:
Short-Term aims:
- Develop high level metrics for reporting on the Eye Care programme
- Develop Model Health System compartments for wide range of benchmarking and monitoring metrics for Eye Care
- Identifying gaps in the data and exploring options to fill these gaps
Longer-Term:
- In-depth benefits realisation / evaluation of the different strands of the programme
- Proof of concept work with local systems to develop metrics where there are gaps in data (e.g. patient experience)
Eyecare Electronic Referral System (EeRS)
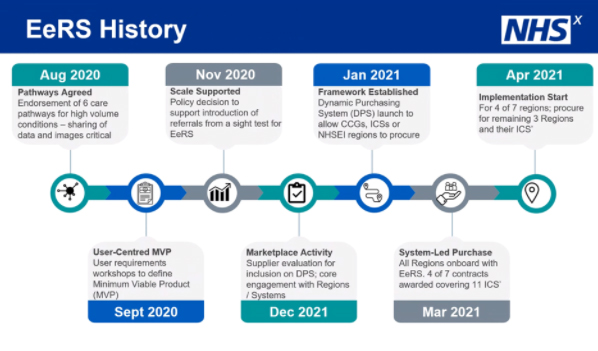
The EeRS workstream is probably most advanced with work commenced under the national outpatient transformation programme and it now becoming a workstream within the new programme. It is expected to work closely with pathway implementation and digital hubs, in particular.
The objective is to scale the use of electronic referral management and image sharing solutions for all eye care referrals across primary and secondary eye care services in England.
A Dynamic Purchasing System was established for electronic eye care referral systems? (ADD LINK TO LOCSU BRIEFING DOC). There are now 13 suppliers on the Dynamic Purchasing System, with 6 having been awarded a contract to deliver EeRS following local procurement.
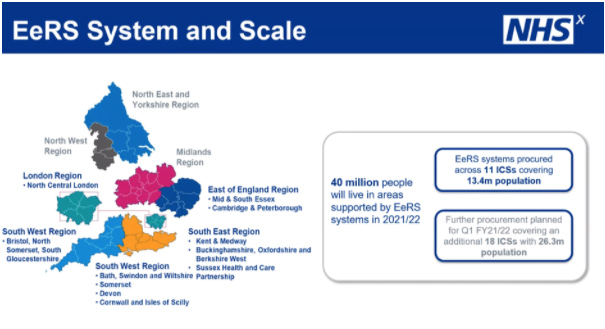
Implementation has commenced across 11 systems within 4 of the 7 NHS regions. Two regions in the North have chosen to re-procure, whilst the Midlands region delayed procurement some months ago.
Each ICS will identify at least one Trust and a number of optical practices to become early adopters. In the early adopter phase referral numbers are likely to be in single digits as they test and embed the process with a view to scaling at pace later in the year.
The slides below provide a helpful summary (April 2021):
NHSE/I plan to set up an EeRS Primary Care Stakeholder Engagement group to bring together representatives from the Primary care optical sector across England in a forum focussed on the EeRS programme implementation.
The group will enable stakeholders to discuss progress and emerging issues from the perspective of primary care optometry, including but not limited to implementation, technical architecture and standards, business change and benefits management, and clinical pathways and safety.
The program is expected to run through 2021 with results being seen in the first half of the year. LOCSU will update all LOCs routinely and relevant documentation relating to the project will be hosted at:
https://www.locsu.co.uk/recovery-reform/
April 2021.